

This evidence has made immunotherapy a clinically validated and effective therapeutic option for some tumors such as NSCLC, melanoma and RCC. In recent years, clinically significant progress in clinical practice resulting in improvements in prognosis of patients with advanced disease was observed thanks to the development of monoclonal antibodies specifically targeting PD-1/PD-L1. However, to date, other immune checkpoints were identified, and some of them could be implicated in immune attacks against cancer. 1), which determine an increase in the progression-free survival (PFS) and overall survival (OS) compared with classical chemotherapy in cancer patients.
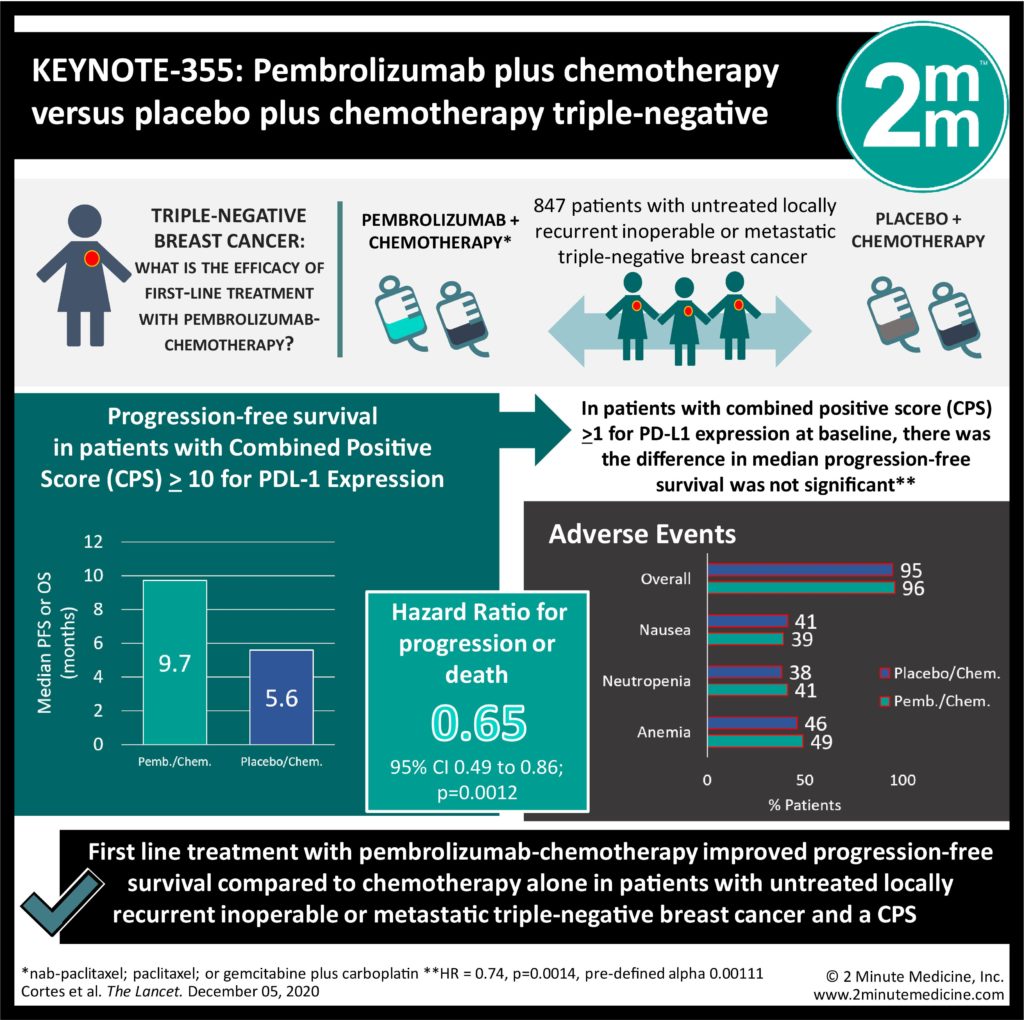
The activity of specific antitumor T cells may be restored via the checkpoint blockade using anti-PD-1 and anti-PD-L1 antibodies (Fig. Therefore, tumors with increased expression of the PD-1/PD-L1 axis show a poorer prognosis. This binding blocks the T cell activation signal induced by the interaction between MHC and TCR by leading to the apoptosis of T cells and preventing targeting of tumor cells and production of cytokines. The activity of T cells may be inhibited by the interaction of the programmed death 1 (PD-1) receptor, an immune checkpoint mainly expressed on the surface of activated T cells, with one of its specific ligands, PD-L1 or PD-L2, expressed on tumor cells. Tumor cells use this mechanism, which leads to the inactivation of tumor-infiltrating lymphocytes (TILs), to circumvent the immune surveillance and survive. The anti-tumor function exerted by the immune system through killer and proinflammatory immune cells may be repressed by the binding of some surface receptors, called immune checkpoints, with specific ligands located on cancer cells. The anti-tumor immune response induction needs three major activation signals that involve (1) the interaction between molecules with co-stimulatory function on antigen-presenting cells (APCs) and receptors present on T lymphocytes (2) the link between tumor-associated antigens (TAAs) exposed by major histocompatibility complex (MHC) and T-cell receptor (TCR) finally, the production of inflammatory cytokines such as interleukin-12 (IL-12) and type I IFN (IFN alpha/beta). The tumor microenvironment (TME) of these tumors is characterized by the abundant presence of several immune cells, including macrophages and T lymphocytes, which, if adequately activated, release cytokines, interleukins and growth factors. Although further studies are currently ongoing, until now, immunotherapy has been shown to be an effective and helpful therapeutic option mainly for some tumors considered generally more immunogenic, including non-small-cell lung cancer (NSCLC), melanoma and renal cell carcinoma (RCC). Recently, much evidence and numerous clinical studies have shown the key role exerted by the immune system in determining an anti-tumor response in cancer patients, allowing the development of multiple therapeutic approaches aimed at stimulating and strengthening this important immune activity system. In this review we will discuss the key role of PD-L1 as a predictive biomarker of response to pembrolizumab therapy in NSCLC patients by describing the appropriate techniques and methodologies for immunohistochemical evaluation of PD-L1 expression and providing an overview of the clinical studies supporting its predictive significance. PD-L1, whose expression is evaluated by using immunohistochemistry analysis, is currently the only biomarker approved for clinical use in the first- and second-line monotherapy setting and therefore plays a central role in treatment decision-making for patients with advanced NSCLC. In particular, NSCLC patients with high tumor PD-L1 levels (proportional score ≥ 50% for first-line therapy and ≥ 1% for second-line treatment, respectively) showed better response rates to immunotherapy and longer survival in first-line therapy compared with conventional chemotherapy.
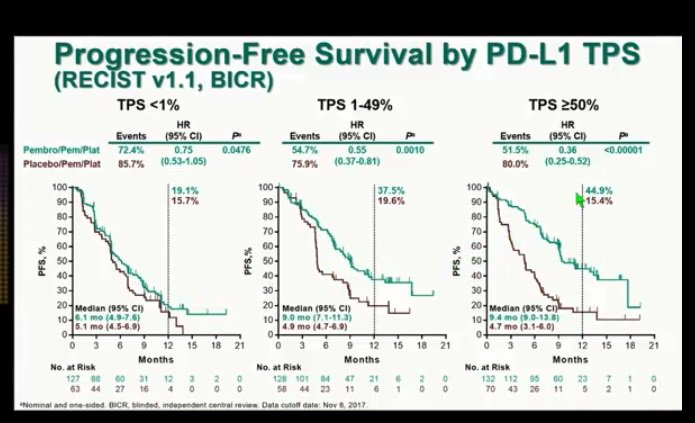
As recently shown by several studies, the PD-L1 expression levels in tumors may offer a selection criterion for patients to predict their immunotherapy response. The activity of antitumor T cells may be restored through the checkpoint blockade using anti-programmed death 1 or anti-programmed death ligand 1 (PD-L1) antibodies, showing, in several cancer patients, an increased progression-free survival and overall survival compared with classical chemotherapy. Recently, immunotherapy has been shown to be an effective and helpful therapeutic option for the treatment of advanced non-small-cell lung cancer (NSCLC).


 0 kommentar(er)
0 kommentar(er)
